Potty training. This is definitely one of the things that did not cross my mind when I was making my…
Browsing Tag:
Crohn’s disease
-
-
Regardless of whether you have been talking about surgery for a long time, putting it off for just as long,…
-
I have mixed emotions about Mother’s Day. Part of me sees the immense value of taking time to thank and…
-
6 years. That’s how long it has been since I have been living with an ostomy. That’s close to 20%…
-
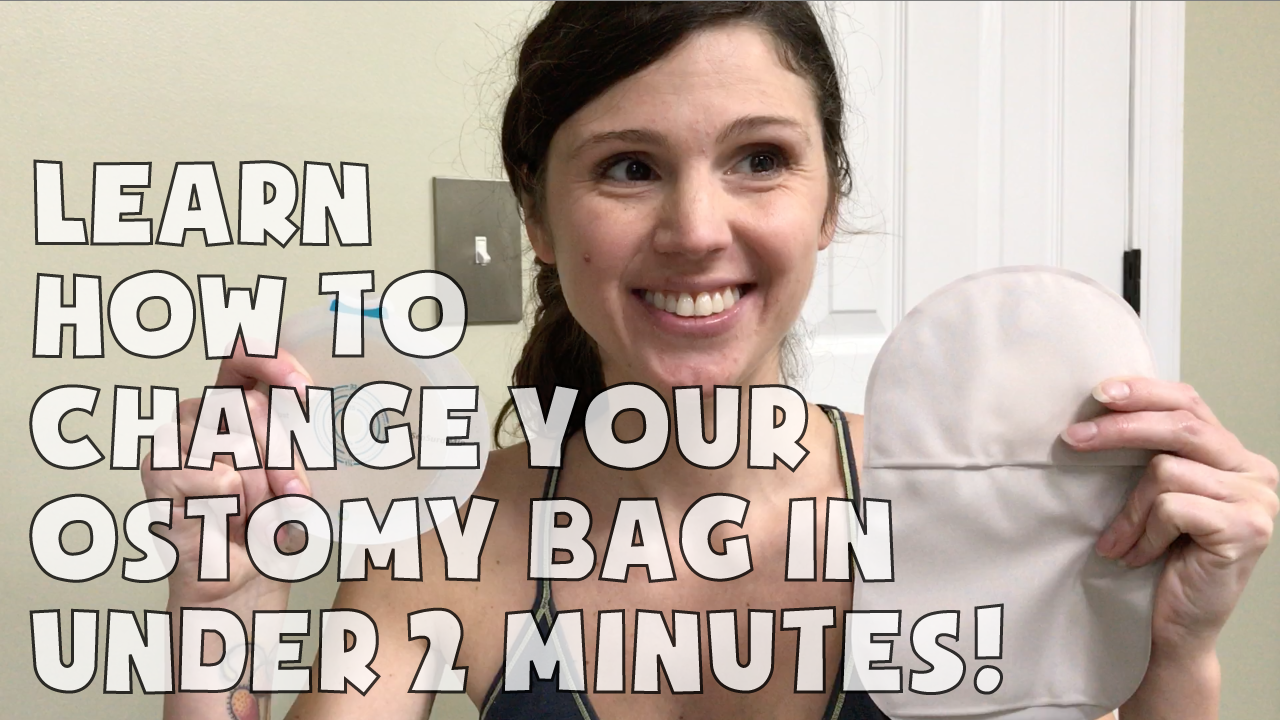
This video is meant to show in under 2 minutes how to change an ostomy bag and the speed of…
-
Everything anyone ever told me about having two kids is true. The past few weeks since the birth of my…