If you talk to 3 different people with an ostomy, they may all actually be living with something very different from the others. As we discussed in our first Ostomy 101 lesson, an ostomy is essentially a non-natural opening in your body by which a person releases waste, but there is more than one type. The type of ostomy is dependent on what part of the digestive tract is used to make the stoma.
Ileostomy: This type of ostomy is made with a part of the small intestine (or ileum). It may be 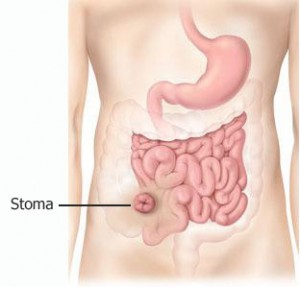 used when the entire colon has been removed (like mine) or it may be temporary following a resection or to allow the colon to heal before being reconnected. It is commonly used in patients with ulcerative colitis, Crohn’s disease, Familial Polyposis (FAP) and colon cancer. It is most often located at the lower right side of the stomach.
used when the entire colon has been removed (like mine) or it may be temporary following a resection or to allow the colon to heal before being reconnected. It is commonly used in patients with ulcerative colitis, Crohn’s disease, Familial Polyposis (FAP) and colon cancer. It is most often located at the lower right side of the stomach.
The poop is usually in liquid form and can be water or more of the consistency of applesauce. The individual does not have any control on the activity of the ostomy and must wear an ostomy bag, which needs to be emptied approximately 5-8 times a day.
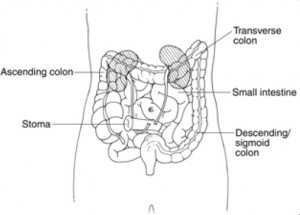
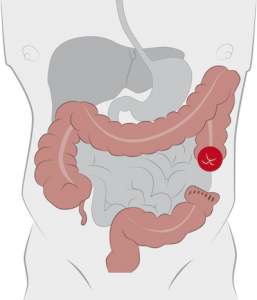 Colostomy: This ostomy is formed with a part of the large intestine. It is used when only part of the colon is removed or when a section of the colon needs time to rest and heal and can also be either permanent or temporary. It is often used for patients who have diverticulitis, colon cancer, bowel obstruction, paralysis, injury or birth defects. There are 2 common types of colostomy that affects its placement: A transverse colostomy is on the upper part of the stomach and a descending/sigmoid colostomy on the lower left of the stomach.
Colostomy: This ostomy is formed with a part of the large intestine. It is used when only part of the colon is removed or when a section of the colon needs time to rest and heal and can also be either permanent or temporary. It is often used for patients who have diverticulitis, colon cancer, bowel obstruction, paralysis, injury or birth defects. There are 2 common types of colostomy that affects its placement: A transverse colostomy is on the upper part of the stomach and a descending/sigmoid colostomy on the lower left of the stomach.
The poop for the transverse colostomy is similar to the ileostomy, but somewhat more formed. The individual does not have control over the activity and must also wear an ostomy bag. For the descending colostomy, the poop is much closer to what is considered normal. The individual sometimes has control over the ostomy activity and may not need to wear an ostomy bag. In this scenario, they would wear a cap of some sort. They also have the option of “irrigating” their ostomy which is essentially an enema through the stoma.
 Urostomy: This type of ostomy is used for the urinary tract. It is actually a little more complicated than the other types of ostomies as it requires the removal of the bladder, as well as a section of the small intestine. The intestine is sewn back together, but the piece that was removed is then attached to the ureters that extend from the kidneys and is also used the create a stoma. It is only done as a permanent solution. A urostomy is most often needed due to bladder cancer, but also inflammation of the bladder or birth defects. It is usually placed on the right side of the stomach.
Urostomy: This type of ostomy is used for the urinary tract. It is actually a little more complicated than the other types of ostomies as it requires the removal of the bladder, as well as a section of the small intestine. The intestine is sewn back together, but the piece that was removed is then attached to the ureters that extend from the kidneys and is also used the create a stoma. It is only done as a permanent solution. A urostomy is most often needed due to bladder cancer, but also inflammation of the bladder or birth defects. It is usually placed on the right side of the stomach.
The pee empties into an attached urostomy bag. The individual has no control over its release. It needs to be emptied approximately every 2-4 hours.
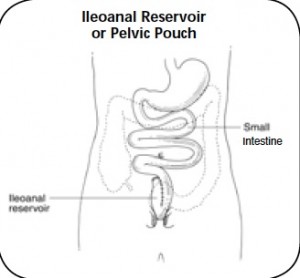 J-pouch: While not a type of ostomy, I feel the need to write a quick summary of a j-pouch. It is made after the removal of the colon when the small intestine can be reattached to the rectum and anus, forming an ileoanal reservoir. This surgery is usually done in 2 stages and involves the creation of a temporary ileostomy. It is often used in patients with ulcerative colitis (but not Crohn’s disease) and FAP.
J-pouch: While not a type of ostomy, I feel the need to write a quick summary of a j-pouch. It is made after the removal of the colon when the small intestine can be reattached to the rectum and anus, forming an ileoanal reservoir. This surgery is usually done in 2 stages and involves the creation of a temporary ileostomy. It is often used in patients with ulcerative colitis (but not Crohn’s disease) and FAP.
In this scenario, the individual can still go to the bathroom in the normal fashion, however, the poop is less formed than what is considered normal.
So now you know: When someone is talking about ostomies, they will most often use “colostomy” as a blanket term, but that is likely to be an inaccurate description. Don’t be afraid to ask somebody you know about theirs. We appreciate not being lumped into a particular group, especially when each type affects individuals differently.
This is a very brief overview of the types of ostomies and there is a TON more that goes into each of these, but it’s a lot more detail than for my purposes here. UOAA has some guides with lots of good information. Images were stolen from here, here, here and here, respectively.


10 Comments
Is it normal to still experience some pain inside my body after having 8 hour ileostomy surgery 6 months ago ?
July 2, 2016 at 2:21 amI also experience some pain 2 days a week when removing my bag to change it my skin in the area where bag is still a little tender ?
Thank for any advice
I have an existing urostomy that was done in 2005. I now need to have a colostomy. Will I have to manage 2 bags ?
September 22, 2016 at 5:32 pmI have thw same question only in reverse. I have a permanent colostomy and am concerned I may need an apr, and have read sometimes this requires removal of the bladder. Do people have 2 bags or is it combined? How does one live this way?
March 27, 2018 at 12:51 amMy dad had an illeostomy and how would
June 26, 2017 at 4:49 amHe pooped
I am now more knowledgeable about which ostomy I have. My doctor’s used the word colostamy but I saw on a report that it was an iliostomy. However, I thought they took most of my large intestines. Also, it depends on what I eat as to the make up of my discharge. I was told I could eat anything as long as I chewed my food thoroughly. So far everything is great!
July 15, 2017 at 11:26 pmI am having a difficult time keeping my pouch from breaking loose at the top. Does not drain and mustaches up at the stomach. Does anyone have Sandy suggestions what I can do to eliminate this problem
February 4, 2018 at 11:05 pmMy mom is 66 and had a colostomy 2 months ago. She doesn’t have appetite and hardly gets out of bed. she say’s she’s fine but hardly communicates with any one. We don’t know what to do to help. Please any advice?
March 8, 2018 at 6:50 amHi Gloria, I’m sorry to hear that your mother is having some difficulty adjusting. It’s so hard early on, but I think it’s so great that you are looking for ways to help! Do you know if there are any support groups in the area? Around me, there is a group you can reach out to and they will send someone from the group to talk to people who have just had surgery. That’s what made the biggest difference for me was just getting to meet someone else who had been through it and could provide some advice and understanding. I would definitely start there. If there’s not, is she someone that might consider joining an online group? Honestly, I feel like getting to know others and joining a community is one of the biggest steps to coming to terms with all of this. Let me know if there’s more I can do. You can also email me at stephanie@stolencolon.com to chat more.
March 12, 2018 at 2:47 pmThank you for being so candid. I have a (new) friend with a “joey”, her term not mine. This article has helped me understand the situation better, without her having to go into embarrassing details. She will talk about it but I cannot make intelligent comments because of my ignorance. So once again, thankyou
May 13, 2018 at 1:06 pmRuby, I am so glad you found it helpful. I think it’s so wonderful that you’re looking into more on ostomies for your friend. We need more people like you in the world!
May 13, 2018 at 6:18 pm